For Referring Providers
An Open Letter and Invitation to Mental Health Providers in Sonoma County
Dear colleagues,
Having moved to Sonoma County from the East Bay in 2016, I am still in some ways new to this area. I'm writing this letter to introduce myself and to help raise awareness of one of the most important things I have discovered in twenty years of passionate study of mental health care. I want to share a little bit of what I know about neurofeedback.
Despite neurofeedback's great power and efficacy, it is still largely omitted from graduate school curricula, and often simply unknown to mental health providers. But because side effects are minimal and results are so durable (1), it should actually be the referral of choice, before medication, in the majority of cases. Particularly if we aim to "first do no harm."
For anxiety or insomnia for instance, we know that benzodiazepines are hugely problematic, and anxiolytics in general have too broad an action (2). While they quiet fear, they also dampen learning and memory (faculties that are often already compromised due to trauma), and effectively shut down progress in psychotherapy (3).
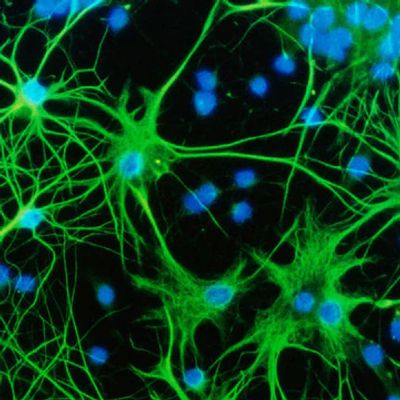
In contrast, neurofeedback works with and enhances brain plasticity (4), and has a beautiful synergistic effect with the therapeutic process. Your clients will blossom. We see this over and over. My therapist consultees who are learning to do neurofeedback are amazed at how much and how quickly their clients transform with neurofeedback.
Similarly, and sadly, we know for certain now that the stimulants prescribed to children with attention issues don't actually create any lasting change, and do measurably stunt growth (5). What could be more opposite from therapeutic intent than stunting growth?
In the case of insomnia, so-called sleep medications only offer sedation or amnesia. Sedation actually disrupts proper sleep architecture, preventing or reducing time spent in the critical restorative stage of deep, slow-wave sleep. Why not offer people an actual therapy for the nervous system instead of just settling for sedation?
And finally, with depression, neurofeedback starts to work immediately to significantly relieve symptoms and brighten mood. Within weeks or months the effect is robust and lasting. Antidepressant efficacy, on the other hand, is lukewarm at best (6). When they do "work" they take weeks to take effect, they may cause further disregulation, exacerbate suicidality, and withdrawal is often prolonged and difficult (7).
I urge you to inform yourself about neurofeedback so that you can make your clients aware of their alternatives and ensure that they can choose from the best available therapies.
I welcome any mental health provider who is interested to come to my office for a visit! I can show you the equipment in person and give you a better sense of the process and experience of neurofeedback for the client.
In service,
Silvia
References
1. Ros T, Baars BJ, Lanius RA and Vuilleumier P (2014). “Tuning pathological brain oscillations with neurofeedback: a systems neuroscience framework.” Front. Hum. Neurosci. 8:1008. doi.org/10.3389/fnhum.2014.01008
2. Merz, B. (2016, December 13). Benzodiazepine use may raise risk of Alzheimer's disease - Harvard Health Blog. Retrieved from https://www.health.harvard.edu/blog/benzodiazepine-use-may-raise-risk-alzheimers-disease-201409107397
3. Benzodiazepines are Contraindicated in Post Traumatic Stress Disorder (PTSD) | Benzodiazepine Information Coalition. (2019, January 5). Retrieved from https://www.benzoinfo.com/2016/09/10/benzodiazepines-are-contraindicated-in-post-traumatic-stress-disorder-ptsd/
4. Ros, T., Théberge, J., Frewen, P. A., Kluetsch, R., Densmore, M., Calhoun, V. D., & Lanius, R. A. (2013). Mind over chatter: plastic up-regulation of the fMRI salience network directly after EEG neurofeedback. NeuroImage, 65, 324–335. https://doi.org/10.1016/j.neuroimage.2012.09.046
and
Kluetsch, R. C., Ros, T., Théberge, J., Frewen, P. A., Calhoun, V. D., Schmahl, C., … Lanius, R. A. (2013). Plastic modulation of PTSD resting-state networks and subjective wellbeing by EEG neurofeedback. Acta Psychiatrica Scandinavica, 130(2), 123-136. doi:10.1111/acps.12229
5. Swanson JM , et al. (2017). Young adult outcomes in the follow‐up of the multimodal treatment study of attention‐deficit/hyperactivity disorder: symptom persistence, source discrepancy, and height suppression. J Child Psychol Psychiatr, 58: 663-678. doi:10.1111/jcpp.12684
6. Whitaker, R. (2018, December 6). Do Antidepressants Work? A People's Review of the Evidence - Mad In America. Retrieved from https://www.madinamerica.com/2018/03/do-antidepressants-work-a-peoples-review-of-the-evidence/
7. Karter, J. (2016, July 30). Study Examines Experience of Long-Term Antidepressant Use. Retrieved from https://www.madinamerica.com/2016/08/study-examines-experience-of-long-term-antidepressant-use/
8. Pigott, E. (2017). The Crisis in Psychopharmacology Provides an Opportunity for NeuroRegulation Treatments to Gain Widespread Acceptance. NeuroRegulation, 4(1), 28-36. doi:10.15540/nr.4.1.28